*The below article, Gingivitis vs Periodontitis: What’s the difference?, is a sponsored post. *
Gingivitis vs Periodontitis: What’s the difference?
The real question is Gingivitis vs Periodontitis: What’s the difference? when talking about dental diseases. Our mouths, teeth, and gums are among our most precious resources. There isn’t a person alive who doesn’t use these tools daily to talk, eat or drink; not to mention whistle, smile, kiss and countless other activities. So if you have swollen, puffy gums or feel tenderness and sensitivity to the touch, your day just got a great deal worse.
Most people have heard the dental terms gingivitis and periodontitis, but would be hard-pressed to describe the difference between the two. And a lot of dental professionals have difficulty explaining how they vary in ways a person can understand without feeling beat up and chastised. Both gingivitis and periodontitis are preventable and treatable once you know what you are up against.
Gingivitis
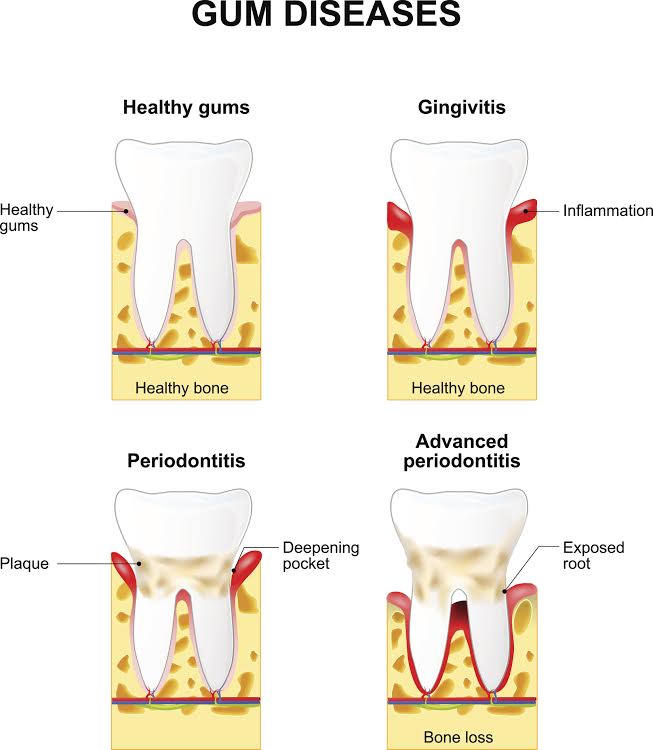
Gingivitis is the most common reason for your swollen and sore gums. In short, gingivitis comes from plaque build-up on your teeth, which inflames your gums causing them to swell and feel tender. You may notice blood when you brush your teeth or bad breath in addition to the tender and swollen gums.
There are scientific ways to describe plaque, but suffice it to say that plaque is the clingy residue of everything that goes into your mouth. Since it is next to impossible to stop eating and drinking, the plaque is hard to avoid. However, dental hygiene can help reduce it. Thoroughly brushing your teeth and gums twice a day and flossing will remove a significant amount of the plaque before it becomes a problem.
Taking care of your teeth with proper cleaning techniques will help to alleviate the discomfort of swollen and bleeding gums from gingivitis. And, although untreated gingivitis does not necessarily lead to periodontitis, also known as gum disease, diligent dental care will go a long way in preventing periodontitis, as well.
Periodontitis (Gum Disease)
While gingivitis can be irritating, it rarely causes long-term damage to your gums or teeth. Periodontitis, however, can lead to long-term tissue and bone damage. You may even lose one or more teeth from infected gum tissue. Periodontitis is not something to ignore. However, many people do not even notice the signs of periodontitis until it is very advanced.
Periodontitis usually begins similarly to gingivitis. Sticky plaque builds up in your gums to such a point that your immune system starts to have trouble fighting the bacteria. Also, other factors can contribute to gum diseases, such as hormonal change, certain medical diseases such as cancer and diabetes, some medications, and even smoking.
Regardless of how it begins, periodontitis leads to an infection in your gums and mouth tissues, often causing puss, bad breath, mouth sores, and red, inflamed gums. If left untreated, your gums will pull away from your teeth, damaging the supporting bones and tissue and creating what are called pockets around your teeth. The pockets allow more bacteria to grow, and the periodontitis to progress. The consequences of gum disease can be loose teeth, a change in your bite, and, eventually, lost teeth.
Treatment Options
Gingivitis and early onset gum disease can often be reversed by visiting a dentist for one or more thorough cleanings and following up with good dental hygiene at home, including brushing and flossing regularly.
More advanced periodontitis, however, needs more aggressive treatments. There are several that can treat gum disease and help you to avoid losing your teeth or damaging your bite:
Scaling and Root Planing – A deep cleaning method, this is a non-surgical procedure whereby your dental professional removes plaque and tartar buildup below the gumline and then planes down the roots so that they reattach to the clean gums.
Occlusal Adjustment – If the gum disease caused your bite to change, an occlusal adjustment could help readjust your teeth and repair your bite. An occlusal adjustment may involve reconstruction, the use of mouth guards, or braces, depending on the nature of the problem.
Flap Surgery – If other treatments do not rid the gums of the infection, your doctor may separate your gums from your teeth temporarily and fold them over (the flap) to get in to clean the roots and bones surrounding your teeth.
Bone and Tissue Grafts – Grafts of either natural or manufactured bone can help to regrow bone and gum tissue that you might have lost to gum disease.
Seek Qualified Help
If you have been diagnosed with or suspect that you have gingivitis or periodontitis, review your dental regime at home and look for ways to improve it. However, that may not be enough. Find a dental professional that you trust to examine the things you can’t see and recommend if a further course of action is needed.
The doctors at King of Prussia Periodontics & Dental Implants are highly trained and up-to-date on the latest care and options for treating gingivitis and periodontitis, both surgical and nonsurgical. Dr. Marissa Crandall Cruz, has a double Masters in biomedical science and oral biology in addition to her MD. Dr. Mana Nejadi has earned specialty training in Periodontics, Implant Dentistry, and Esthetics and served as the Director of the Predoctoral Periodontics program at the University of Pennsylvania between 2013 and 2015. Dr. Rimple Sandhu received her certificate in Periodontics at the University of Pennsylvania School of Dental Medicine, and is knowledgeable and experienced in both surgical and nonsurgical periodontal treatment.
All three doctors and the entire staff are committed to providing relaxing, comfortable attention and strive to provide their patients a compassionate, non-judgemental treatment environment. Visit King of Prussia periodontics & Dental Implants at https://www.kopperio.com or give them a call at (610) 783 7800.